A Balanced Heart Is A Healthy Heart
Are you living from the heart? Find out. Take our brief quiz to get your own #LiveFromTheHeart tip sheet.
Take the quiz!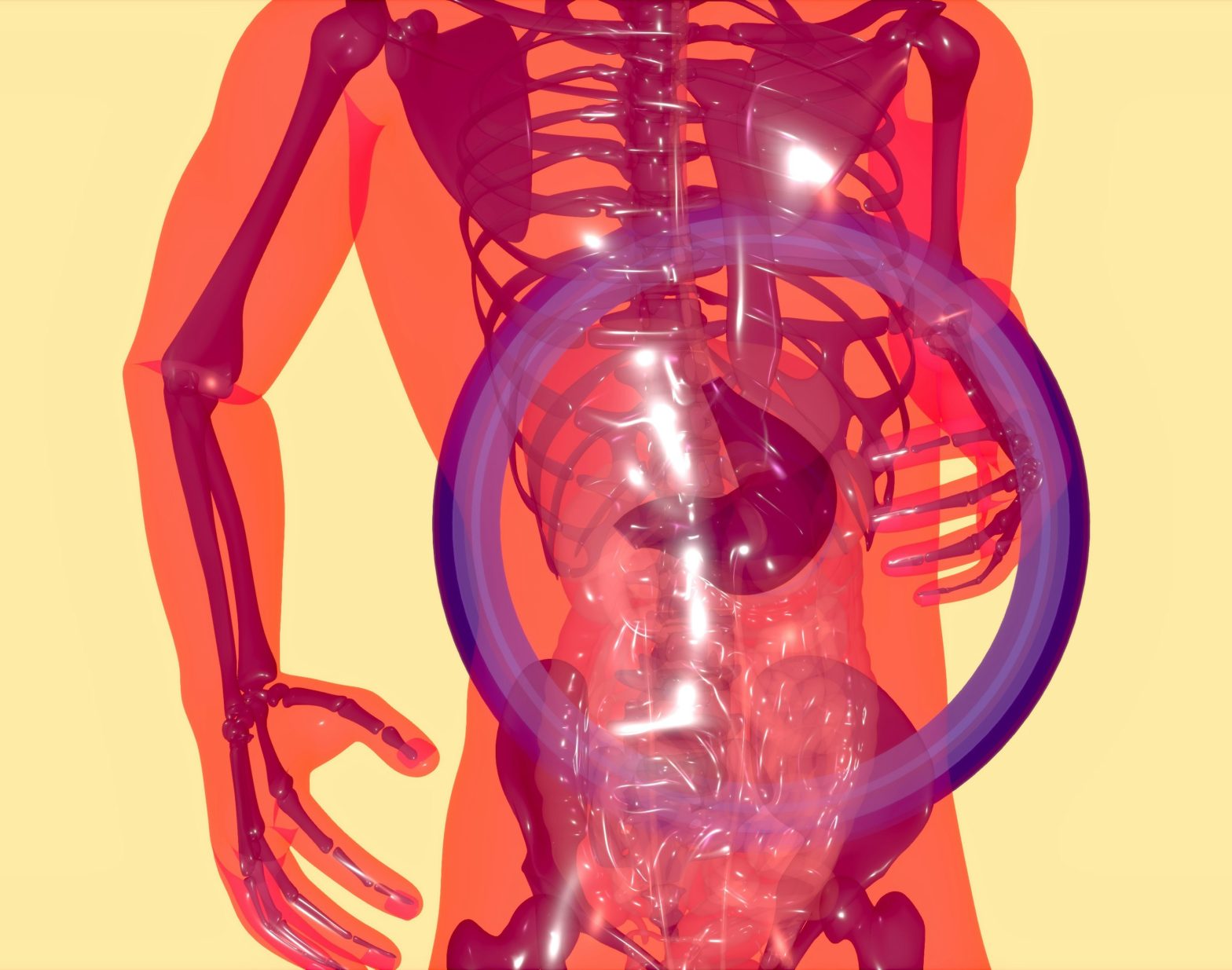
By FemGevity Medical Team | Posted Sep 26, 2024
Menopause is a natural biological process that occurs in women, typically between the ages of 45 and 55, marking the end of their reproductive period. Symptoms of perimenopause can begin as early as 10 years before menopause meaning women may start feeling symptoms related to perimenopause and menopause as early as 35. During this transition, women experience a range of physical and emotional symptoms, including hot flashes, night sweats, mood swings, rage, depression, anxiety and vaginal dryness. While menopause is a normal part of aging, its symptoms can significantly impact a woman’s quality of life.
Recent research has highlighted the importance of the gut-brain connection in menopausal health. The gut microbiome and even something called the estrobolome, composed of trillions of microorganisms, plays a crucial role in regulating various physiological processes, including hormone metabolism, immune function, and brain health. The estrobolome is a portion of the gut-micobiome bacteria that metabolize estrogen and when not functioning properly can affect estrogen metabolism and estrogen breakdown. Changes in the gut microbiome during menopause can impact the perception of symptoms and can affect overall health.
The gut microbiome produces metabolites that can influence hormone levels and activity. During menopause, the decline in estrogen levels can lead to changes in the gut microbiome, which in turn can affect hormone metabolism and exacerbate menopause symptoms. For example, the gut microbiome can convert estrogen into its more potent form, estradiol, through the action of enzymes like beta-glucuronidase, which can then be reabsorbed into the bloodstream, contributing to hot flashes and other symptoms.
Conversely, changes in the gut microbiome can also influence hormone levels. For instance, certain gut bacteria, such as Lactobacillus and Bifidobacterium, can produce short-chain fatty acids that can stimulate the production of estrogen and progesterone. This complex interplay between hormones and gut bacteria highlights the importance of considering the gut-brain connection in menopausal health
Studies have shown that menopause is associated with significant changes in the gut microbiome. One study published in the journal Nature Communications found that menopausal women had lower gut microbiome diversity and a shift toward greater similarity to men in microbiome composition. This shift was characterized by an increase in Firmicutes and a decrease in Bacteroidetes, which can lead to changes in hormone metabolism and immune function.
Another study published in the Journal of Clinical Endocrinology and Metabolism found that menopausal women had higher levels of Escherichia coli and Streptococcus in their gut microbiome, which can contribute to inflammation and oxidative stress.
Gut bacteria play a crucial role in estrogen metabolism, and changes in the gut microbiome during menopause can affect estrogen levels and activity. For example, certain gut bacteria, such as Clostridium and Eubacterium, can convert estrogen into its more potent form, estradiol, which can then be reabsorbed into the bloodstream, contributing to hot flashes and other symptoms.
Additionally, gut bacteria can influence the expression of estrogen receptors, which can affect the body’s response to estrogen. For instance, Lactobacillus and Bifidobacterium can increase the expression of estrogen receptor alpha, which can lead to improved estrogen signaling and reduced menopause symptoms.
A study published in the journal Scientific Reports used 16S rRNA gene sequencing and functional prediction analysis to investigate the gut microbiome of menopausal women. The study found that menopausal women had lower gut microbiome diversity and a shift toward greater similarity to men in microbiome composition.
The study also found that menopausal women had higher levels of Firmicutes and lower levels of Bacteroidetes in their gut microbiome, which can lead to changes in hormone metabolism and immune function. Functional prediction analysis revealed that menopausal women had higher levels of genes involved in estrogen metabolism and lower levels of genes involved in immune function.
While the studies discussed above provide valuable insights into the gut-brain connection in menopause, there are still significant research gaps that need to be addressed. For example, more research is needed to understand the mechanisms by which the gut microbiome influences hormone metabolism and menopause symptoms.
Additionally, further studies are required to investigate the potential benefits of targeting the gut microbiome for the prevention and treatment of menopause-related symptoms. This could include investigating the effects of probiotics, prebiotics, and other nutritional interventions on the gut microbiome and menopause symptoms.
The gut-brain connection in menopause highlights the potential for gut microbiome regulation to improve menopausal health. This could include:
The gut-brain connection in menopause highlights the potential for harnessing the gut microbiome to improve menopause symptoms and health outcomes. This could include:
Balancing the gut microbiome doesn’t just lead to better bowel movements; it can also have a profound impact on various aspects of women’s health and well-being. Achieving gut balance can result in:
These beneficial effects stem from the intricate interactions between the gut microbiome, immune system, and various physiological processes throughout the body. Achieving gut balance through dietary and lifestyle interventions can thus yield wide-ranging benefits beyond gastrointestinal health, enhancing overall quality of life during menopause and beyond.
The gut-brain connection plays a significant role in menopausal health, as changes in hormone levels and gut bacteria can influence various aspects of women’s well-being. Understanding the relationships between hormones, gut bacteria, and menopause symptoms can lead to potential techniques for the prevention and treatment of menopause-related symptoms.
Further research is needed to confirm these findings and identify replicable associations of menopause with gut microbiome taxa. However, the existing evidence suggests that targeting the gut microbiome may provide a novel approach to improving menopausal health and reducing symptoms.
By harnessing the power of the gut microbiome, we may be able to improve the lives of millions of women worldwide, providing them with a better quality of life during this critical phase of their lives.
This post first appeared on the FemGevity website in May 2024 and was reproduced here with the permission from the authors.